

For more than a year now, we have been living in a worldwide pandemic. At first, the new conditions were expected to bring changes in various spheres of life. And the changes really took place, but most of them remained invisible to the average person.
By early spring 2021, the SARS-CoV-2 pandemic had become routine. People understand the danger of the disease, and follow certain precautionary rules. One can argue about how rational the introduced measures are, but one point is not in doubt even among the most hardened skeptics. It is very important to detect the disease as early as possible. Therefore, tests to determine the coronavirus infection have become a routine element of modern life. Let's see what they are and how they work.
Speaking about the types of tests for coronavirus infection, it is worth highlighting three groups:
-
- based on the analysis of big data (accumulated statistics);
-
- commonly used laboratory tests;
-
- used only in scientific laboratories.
It is easiest to talk about the first category. This includes diagnostics by clinical manifestations, identification of markers of the disease that are not obvious at first glance, and even very strange ideas, such as detecting a coronavirus infection by the smell of sweat, for which special dogs are trained.
There are quite a few frankly meaningless techniques in this category. Sometimes you can even see applications for smartphones that are supposedly able to determine the disease, for example, by the sound of a cough. (We recommend the article: "Genetic analysis in perinatal diagnostics")
Alas, in medicine, a pseudoscientific approach may not only be useless. It can be dangerous because decisions made on its basis will prevent a person from seeking qualified help in time.
On the other hand, some of these tests really have a basis. But it is important to understand that all of them are only correlational. That is, they do not show the presence or absence of SARS-CoV-2 in the human body. They only indicate the phenomena that often accompany coronavirus infection. Actually, this group of tests can hardly be called such in a strict scientific sense.
Now about the tests that are used in evidence-based medicine. In clinical practice, there are only two types. Determination of the genetic material of the virus in the human body and the determination of antibodies to any component of the virus.
In scientific laboratories, the definition of virus-specific lymphocytes is added to them. This test is somewhat more significant, since it is cellular immunity that is primarily responsible for protecting against viruses. Therefore, this test is necessary in clinical trials. However, it is too long, laborious and expensive to be used to detect the disease in a wide range of potentially ill people.
Further, we will consider only the polymerase chain reaction (PCR), which detects genetic material, and immunological reactions: enzyme-linked immunosorbent assay (ELISA) and microneutralization reaction, used to detect antibodies.
The difference between these two methods is that PCR immediately detects the presence of the virus even at an early stage of the disease. Antibodies, on the other hand, appear only some time after a person becomes infected (incubation period). That is, by antibodies it can be judged that the virus was in the human body some time ago. Whether a person is infected now, immunological tests will not show.
How does the polymerase chain reaction work? PCR is a very ingenious discovery, thanks to which biologists have made a huge number of discoveries over the past decades. This technique uses the mechanisms underlying the very basis of life. Almost exactly the same as it happens in a cell, DNA synthesis occurs in a test tube.
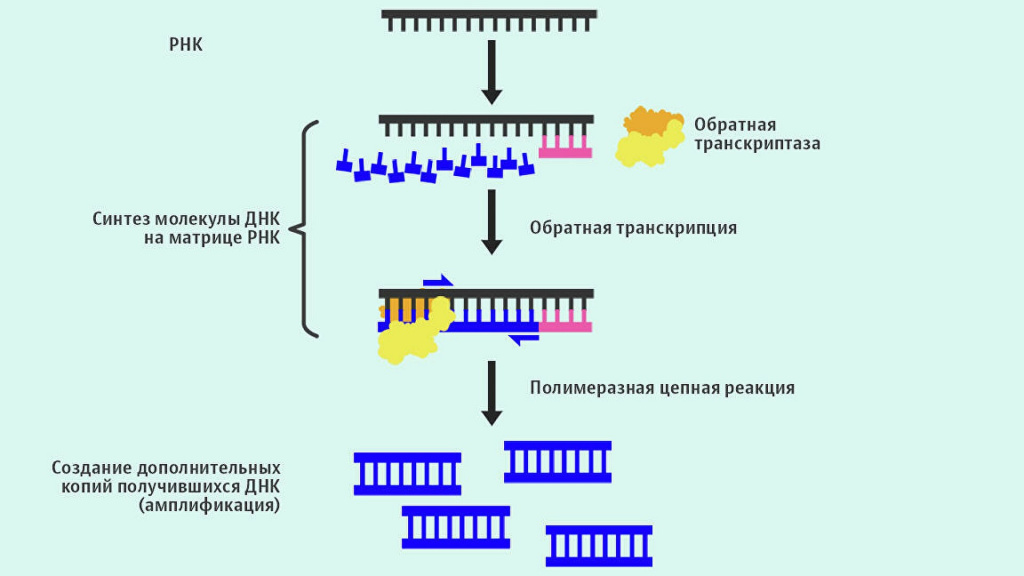
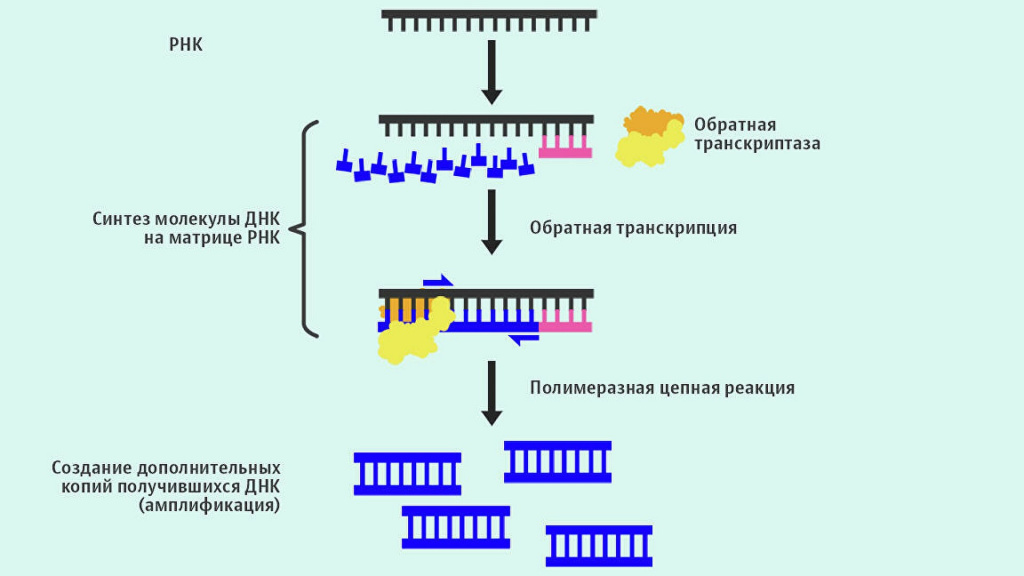
The principle is simple. First, select the section of DNA that you want to detect. In the case of SARS-CoV-2, these are two viral genes. One is characteristic of the coronavirus family, to which the culprit of the modern pandemic belongs, and the second is found only in this particular virus. Once a site has been chosen, two small pieces of DNA need to be synthesized that will specifically (complementary) bind to it. These fragments are called primers, and flank (limit) the region of DNA that will be synthesized in the test tube. In different tests, these can be whole genes, or their parts containing unique sequences that are significant for analysis.
Then the biological material under study (in this case, a wash from the nose or throat) is mixed with the reaction mixture, which includes primers, enzymes and nucleotides - structural units for the synthesis of new DNA.
If the DNA from the material under study contains regions that are complementary to the primers, then a copy of the desired DNA fragment is synthesized during PCR. And then another, and another, and another - exponentially. Each new copy will serve as a template for the synthesis of new DNA segments.
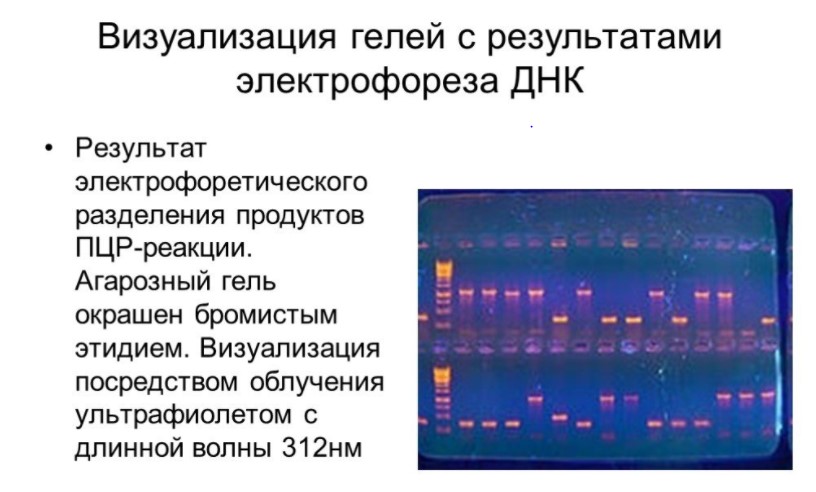
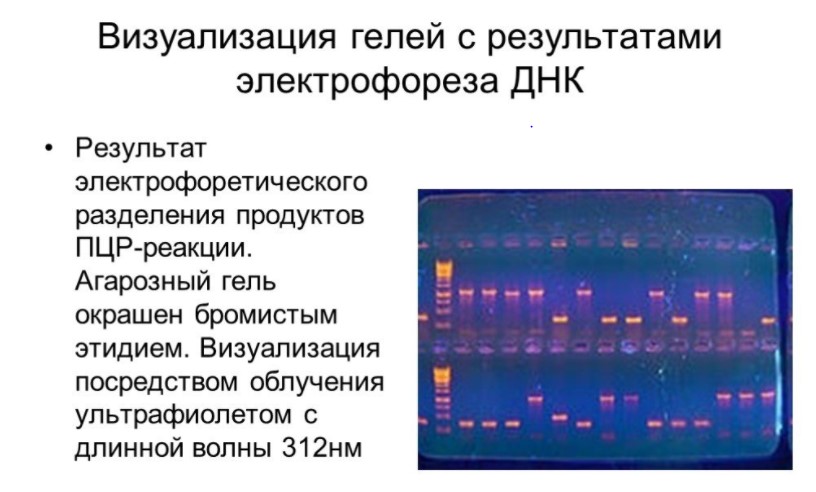
At the end of the reaction, there will be so many of them that the resulting DNA fragments can be seen with the naked eye. To do this, they need to be separated in agarose under the influence of an electric field (phoresis), and then visualized with a dye in ultraviolet light.
However, this method of DNA imaging is rarely used. Modern devices make it possible to estimate the number of fragments directly during PCR - in “real time”. Today, PCR is used to identify kinship, determine the origin of a person, or, for example, clarify biological systematics (kindredness of species).
PCR is a very accurate and sensitive test. It only needs a few copies of DNA. However, this sensitivity can be a weak point of the method. The slightest contamination of the test material with third-party DNA can lead to false positive results. This is especially true in institutions where there are many potentially infected people at the same time (hospitals, clinics).
Viral particles are constantly present in the air, and we are exposed to them every second. Another thing is that the vast majority of such attacks lead nowhere. The virus either fails to get inside the cell at all, or the immune system responds quickly and prevents the virus from spreading inside the body. However, if the virion is deposited on the smear, this may cause an error.
False-negative results do occur, but much less frequently. Their reason is a violation of the analysis methodology, therefore, in case of reasonable suspicion, the test should be redone. The most common reason for reasonable suspicion is a previously confirmed infection.
Now let's analyze the immunological reactions. They are usually of two types: enzyme immunoassay and microneutralization reaction. They have the same principle - blood serum, which may contain antibodies, interacts with the virus or some of its components. If antibodies are present in the serum, they bind to their antigen (target). The differences between the methods are as follows.
In enzyme immunoassay, the component of the virus (antigen) is fixed on a plastic substrate. Antibodies bind strongly to it and the resulting complex is stable throughout the assay. The fixed antibodies are treated with the conjugate. Usually, these are also antibodies with a chemically cross-linked dye. The result is a kind of sandwich, where the antibodies are located between the antigen and the conjugate. (We recommend the article: "Genetic analysis in agriculture")
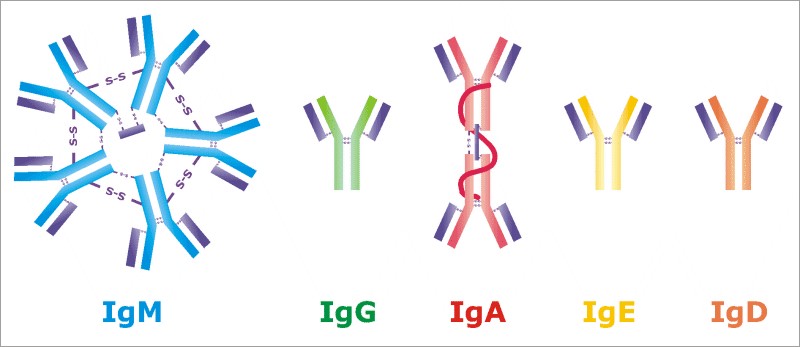
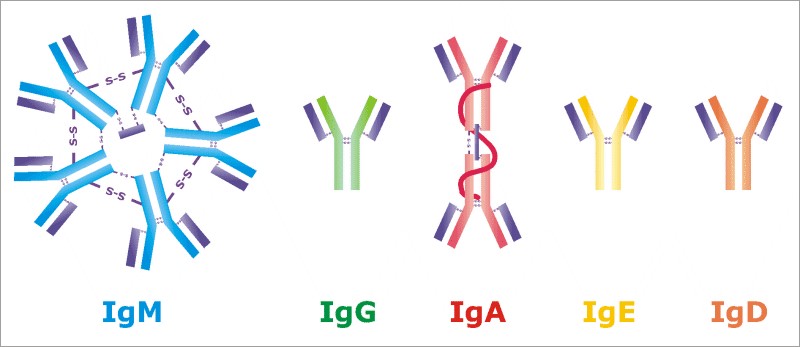
Antibodies are of different types. In this case, we are interested in three: IgA, IgG and IgM. First, IgA are “guardians of the entrance gate of infection”, there are many of them in the mucous membranes, and they are the first to meet the virus. IgG are professional virus hunters. They appear a few days after the onset of the disease, and very accurately recognize their opponent. Each antibody of this type binds to only one site of one substance. IgM are the workhorses. They are constantly present in the blood and do not bind to pathogens as strongly as IgG. But on the other hand, they are not so specific - they can interact not with one specific substance, but with several similar ones.
In the microneutralization reaction, neutralizing antibodies are determined. This is not a separate type of antibody, but a functional category. This method uses an active but weakened virus. If antibodies are present in the test serum, they bind the virus. If there are no antibodies, the virus remains in a free state. Next, the cell culture is infected with this mixture and it is observed whether the cells will die. If everything is in order with the cells, then there is no virus in the sample. And if there is no virus left in the mixture, then the antibodies have neutralized it.
The reaction of micro-neutralization is more indicative of the issue of body protection. But, since living cells and an active virus are used in it, special conditions are required to carry out this reaction. ELISA does not require special conditions. Therefore, the microneutralization reaction usually confirms the results obtained using other methods.
By the way, the very existence of antibodies and the entire system of specific immunity is an indicator that viruses do not always bring only evil. Lymphocytes appear as a result of a process that, without exaggeration, can be called forced evolution. And we got this mechanism thanks to a virus that infected our very distant ancestor. So distant that the most advanced organisms at that time were something like modern starfish. Since then, this virus has been present in our genome, protecting against all sorts of pathogens that can threaten life.


On this optimistic note, we conclude the story about the methods of laboratory diagnosis of coronavirus. Take care of your health and be healthy!.

